Pelvic Organ Prolapse
“Something Feels Heavy Down There — Am I the Only One?”
You might have felt it after standing too long, lifting something heavy, or just going about your day — a heaviness or pressure in your lower body that’s hard to explain. Maybe it feels like something is bulging or falling, and you’ve even checked with a mirror, wondering, “Is something coming out of me?” You’re not imagining it — and you’re not alone.
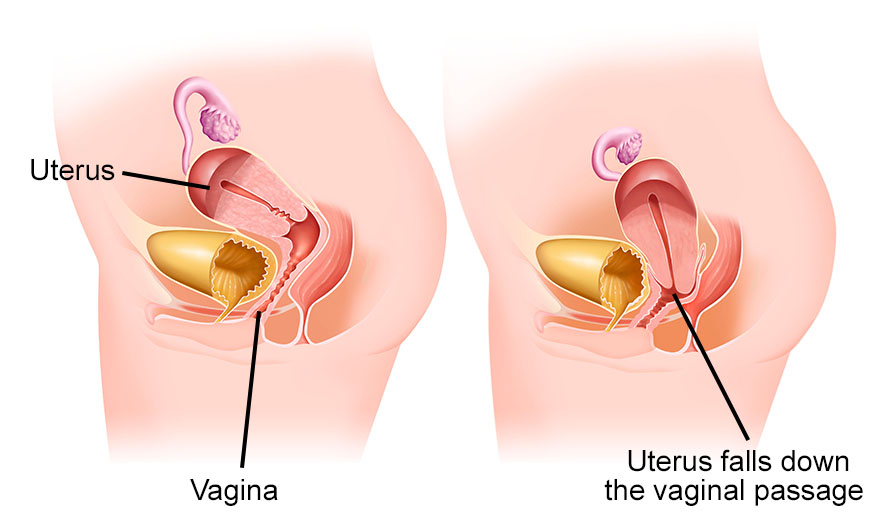
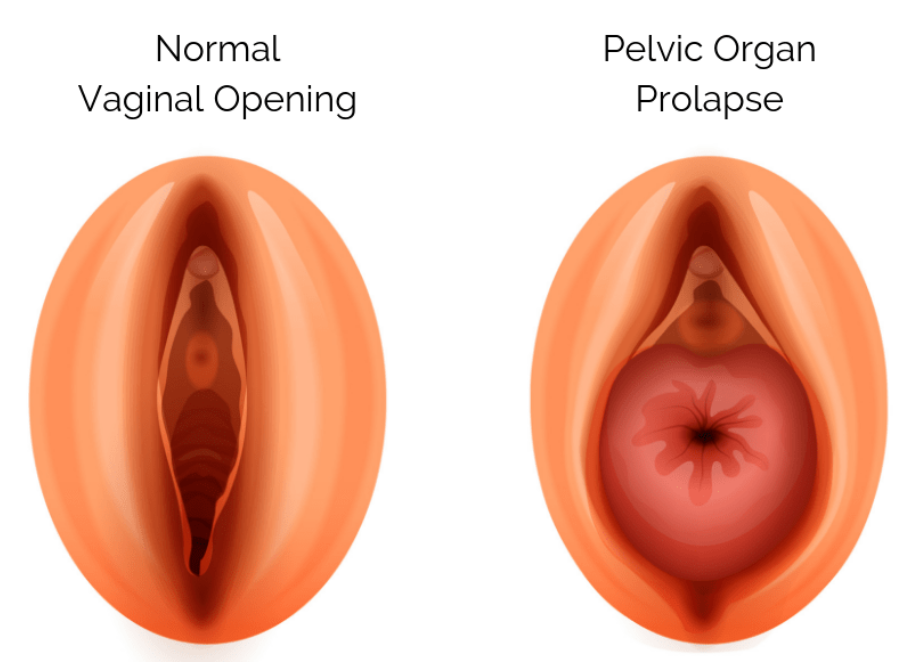
Pelvic organ prolapse occurs when weakened pelvic muscles and tissues allow organs like the bladder, uterus, or rectum to shift into the vaginal space. It may cause pressure, a visible bulge, or discomfort. Though often distressing, support and care are available at Solace.
Pelvic organ prolapse occurs when weakened pelvic muscles and tissues allow organs like the bladder, uterus, or rectum to shift into the vaginal space. It may cause pressure, a visible bulge, or discomfort. Though often distressing, support and care are available at Solace.
Symptoms
Pelvic Organ Prolapse may feel like:
- A heavy or dragging sensation in the pelvis
- Pressure in the vagina
- A visible bulge at the vaginal opening
- Discomfort during standing, walking, or lifting
- Difficulty fully emptying the bladder or bowel
- A feeling of 'something there' when you wipe
These symptoms can be deeply unsettling — not just physically, but emotionally as well. Many women feel confused, fearful, or even ashamed to speak about prolapse, often unsure who they can turn to for support or answers.
You Don’t Have to Be Older or a Mother to Have Prolapse
It’s a common misconception that prolapse only happens to older women, or those who’ve had many children.But we see:
- Women in their 20s and 30s
- First-time mothers
- Women who’ve never given birth
- Fitness enthusiasts
- Women who’ve experienced chronic constipation, heavy lifting, or long-standing pressure in their bodies
You are not too young to be taken seriously.
You are not overreacting.
And you are not the only one going through this quietly.
You are not overreacting.
And you are not the only one going through this quietly.

Treatment May Include
Step 1
Initial Consultation & EducationReviews history and symptoms, introduces a bladder diary, and provides basic education on pelvic floor anatomy and incontinence types.
Step 2
Pelvic Physical AssessmentInvolves postural and movement evaluation, along with internal and external pelvic floor muscle assessment to check tone, strength, coordination, and signs of prolapse.
Step 3
Customized Pelvic Floor Activation TreatmentIncludes individualized pelvic floor muscle training, bladder training tips, advice on toileting posture, and fluid management strategies.
Step 4
PlanningFocuses on establishing short- and long-term goals, outlining follow-up visit frequency, answering questions, and providing take-home educational materials.
A calm, private space where you can speak freely — without fear or embarrassment.
Here, you're seen not just as a patient, but as a whole woman, with feelings, fears, goals, and stories.
You’re not alone — we’re listening, and we’ll face this together.
×
![]()
